Understanding Chronic Kidney Disease
By Dr Anupama De Silva
For many CKD patients, a kidney transplant is the best hope for survival
What is Chronic Kidney Disease (CKD)? It is the gradual, progressive and irreversible loss of kidney function over several months to years. When someone has CKD, kidney function declines continuously and slowly. After a long period, it reduces to a stage where the kidneys stop working almost completely. This advanced and life-threatening stage of disease is called End Stage Kidney Disease (ESKD). In the early stages of CKD, signs and symptoms are minimal. Symptoms appear only when the disease is advanced. Common symptoms related to advanced CKD are weakness, loss of appetite, nausea and vomiting, swelling of the body and generalised itching. Most of these symptoms are non-specific, and unless kidney disease is suspected in the presence of these symptoms, diagnosis of CKD is likely to be delayed.
Is CKD a public health problem in Sri Lanka?

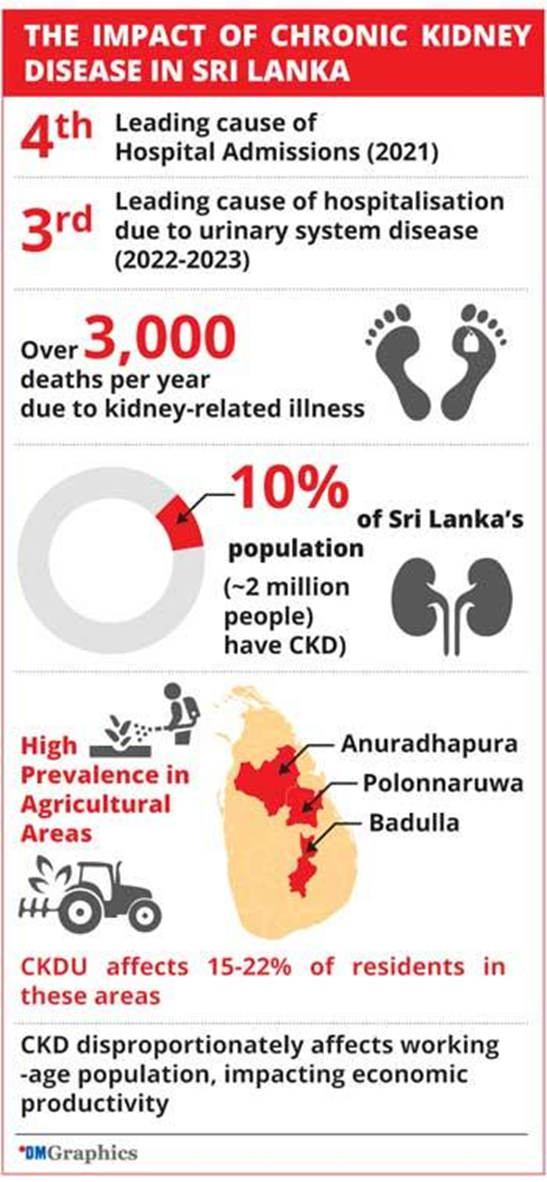
The impact CKD has on Sri Lanka
CKD in Sri Lanka has a big disease burden. The numbers vary from district to district due to the additional burden from so-called ‘CKDu’. Overall, in Sri Lanka, about 10% of the population has CKD. Therefore, we have over 2,000,000 patients with CKD, of which most cases have diabetes mellitus. In the North Central part of Sri Lanka, Anuradhapura, Polonnaruwa and Badulla Districts, in addition to CKD, there is a disease called CKDu (Chronic Kidney Disease of uncertain origin). CKDu has impacted almost 15–22% of the population in those areas. Overall, the kidney burden in these areas is high.
Plans for World Kidney Day and its importance in Sri Lanka
World Kidney Day was founded in 2006 by the International Society for Nephrology to address issues related to kidney diseases. It is marked in the second week of March, and as such, it will be held on March 13. The Day is a global movement to create awareness amongst the public and healthcare professionals on identifying and treating issues around kidney health. Since Sri Lanka has a significant kidney health issue, which has been ongoing for some time, we use World Kidney Day (WKD 2025) to build awareness in Sri Lanka about the related issues.
NINDT plans in lieu of WKD 2025
The National Institute for Nephrology Dialysis and Transplantation (NINDT) is in line with the international theme ‘Are your Kidneys OK?’, and we have planned a series of events. The programme is structured on three principles, The first is to empower and give knowledge to the healthcare staff. The second is to make the public more aware of the risks and treatments. The third was to facilitate the organ donors of Sri Lanka, whom we are thankful for giving the gift of life to others. The felicitation ceremony, the first of its kind, will be held on March 14. There was also a kidney health awareness walk, which was held on March 9 and was centred around NINDT and the locality. As such, we have planned to hold workshops for our doctors, nurses and the para-medical staff during this period. We have planned a few events to build team spirit amongst our staff. The NINDT has also organised a public awareness campaign, which plans to use all forms of media. In the pipeline, there are several awareness-building videos which will include advice from specialists on how to keep your kidneys healthy and safe. They will also address how to plan your treatment with medical advice for those who are already suffering from kidney issues. In the first week of March, NINDT plans to launch a publication on the issue authored by Consultant Nephrologist Dr. Anupama De Silva for kidney patients, which will be published in all three languages.
Who should get their kidneys checked? Who is at high risk for developing kidney problems?
For anyone with diabetes or high blood pressure History of cardiovascular disease (i.e. heart attacks, heart failure, stroke), History of kidney disease, especially with diabetes, high blood pressure and polycystic kidney disease, Living in an area where the chronic kidney disease of uncertain aetiology (CKDu) is endemic, History of structural problems in your genito-urinary tract and recurrent kidney stones, Medications known to impact your kidneys in the long run (i.e. pain killers), History of multi-system/chronic inflammatory condition (i.e. SLE, vasculitis) and any previous episodes of temporary reversible deterioration of kidney function (Acute Kidney Injury) with infections and exposure to certain medications.
Issues related to the quality of groundwater as a factor for CKDu
Yes, groundwater quality has been a contributory factor. This is because in those areas, the groundwater is found to contain heavy metals. It is suspected that most of the heavy metals originated from the unregulated use of certain types of agrochemicals, weedicides and pesticides. The groundwater has been contaminated with Cadmium, Arsenic, etc.
Screening Tools
A urine full report (UFR) is a simple, inexpensive and very useful diagnostic test. Abnormalities seen in the UFR would provide important clues, but a normal report does not rule out kidney problems. The presence of protein in urine (proteinuria) is seen in various kidney diseases. It should never be neglected. Smaller protein leaks in urine may not be detected in a full urine report. Urine Albumin Creatinine Ratio (UACR) is useful to detect significant urinary protein leaks in early stages of CKD. Blood tests measure levels of creatinine, which reflect the function of the kidneys. Creatinine is a waste product removed from the blood by the kidneys. When kidney functions decline, the blood level of creatinine rises. The higher the value, the greater the degree of kidney damage.
The Screening is Done,
What’s Next?
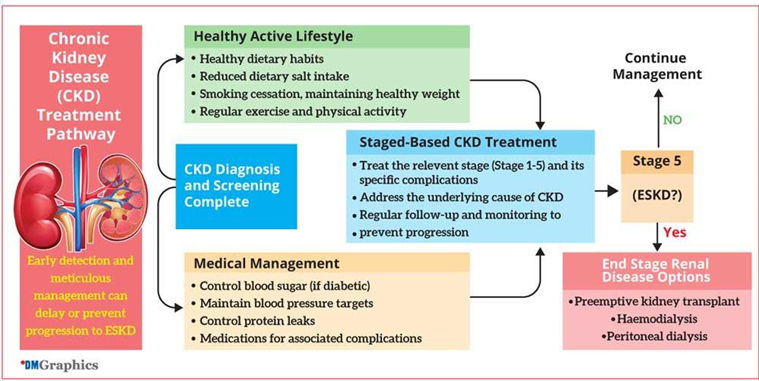
Patients will need to adopt a healthy active lifestyle: Healthy dietary habits, reduced dietary salt intake, stopping smoking, maintaining a healthy weight, exercising regularly and remaining physically active regularly. Achieving prescribed targets of blood sugar and blood pressure control is of utmost importance in patients with diabetes and high blood pressure. Doctors looking after these patients will prescribe medications to treat associated complications and mitigate cardiovascular risks. As these health conditions take a longer time to progress, regular follow-up is needed to ensure a smooth transition to ESKD. Early detection and meticulous management is the only feasible and cost-effective ways to treat CKD and delay the need for dialysis and kidney transplantation.
Once diagnosed, how does treatment work?
Mainly, we can treat the stage of CKD and or treat the causes of CKD. For example, if CKD is caused by diabetes, we treat that and control it. We also control conditions such as blood pressure and control protein leaks. This is to prevent further growth of CKD. There are five stages of CKD. We treat the relevant ailments of that particular stage. The complication of each state needs to be managed while the main cause is addressed. This way, we can manage the situation and improve it without allowing the situation to deteriorate to the level where dialysis or kidney transplantation is needed. Sometimes, depending on the cause, some cases can be 100% treatable. CKD can also be managed to a great extent without letting it progress to the end stage. Despite all these measures, if a patient reaches stage five, the end stage renal disease, there are options to manage the situation. In such cases, there are occasions where we can go for a preemptive kidney transplant without going for the dialysis stage. This is because, in some cases, kidney transplants are the best option for the patient. Where dialysis is needed, there are two types of it. One is hemodialysis, where the patient goes to a center where his or her blood is filtered and cleaned via machine. The other form, peritoneal dialysis, is where a cleansing fluid is passed through a catheter tube into part of the abdomen known as the peritoneal cavity. There are other options of dialysis as well.
How kidney transplantation works
Getting a kidney transplant is a complex process. In Sri Lanka, we have two types of organ donation, live donation and deceased donation, where organs are donated from someone who has passed away. Since we have two kidneys, some people donate one to those in need. The other form of donation, if a parent or families of a brain dead donor is agreeable to it, the deceased kidney can be donated. To receive a kidney donation, a patient has to be prepared to receive it. Since the body will view the new kidney as a foreign entity, the blood groups and relevant HLA protein markers and PRA markers need to be properly matched to the donor organ to ensure success and prevent organ rejection by the host body. Once you get a proper match from a donor, the surgery is rather a simple procedure.
The process of receiving a kidney from a deceased donor
There is a legal process when we use a live donation, where no financial benefit to the donor is allowed. There is a process of ethics and a committee at the hospital, and the Ministry of Health oversee the process to ensure that it is done properly. At the same time, for donations from a deceased donor, the relatives and close family members must be happy to do so and give consent. Only with consent can the organs be harvested. This is carried out by a specialised team at each hospital. The team is led by an anaesthetist. Internationally, there is a declaration on organ trafficking, and we in Sri Lanka adhere to the same guidelines.
Diabetic Kidney Disease (Diabetic Nephropathy)
How common is kidney disease in Diabetic patients? It is estimated that 40% of Diabetics will suffer from kidney disease in their lifetime. It is also interesting to note that Diabetes is the leading cause of Chronic Kidney Disease, which requires Dialysis or Kidney transplantation worldwide.
Screening
Type 1 Diabetics should be screened 5 years after the diagnosis.
Type 2 Diabetics should be screened as soon as they are diagnosed and then yearly after that.
Why does Diabetic Nephropathy occur?
There are a few factors that contribute, but one of the main reasons is persistently high blood sugars, which in turn damage the kidney cells (Glomeruli), which in turn start filtering more protein that is needed for the body. Poor management of blood pressure could be another important factor in the accelerated worsening of a Diabetic Kidney.
Diagnosis
For this, we need to do an Urine Albumin Creatinine Ratio (UACR) and depending on the quantification of protein filtered through the kidney, we classify as either Microalbuminuria (30-300mg/g) or Macroalbuminuria (>300mg/g). This also needs to be repeated and confirmed in 3 months, ideally. Confirmation can be obtained with an Ultrasound scan of the Kidneys.
How do you categorise the severity of Diabetic Nephropathy?
Blood tests for Serum Creatinine and eGFR (estimated Glomerular Filtration Rate) need to be assessed and depending on these findings, your doctor will categorise into separate entities to assess risk and how to manage it going forward. The most commonly used classification is the KDIGO (Kidney Disease Improving Global Outcomes) classification, where there are 5 stages of Chronic Kidney Disease, with Stage 5 being End Stage Kidney Disease, which requires Dialysis or Kidney Transplantation.

Diabetic Nephropathy Prevention
The simple answer to this would be to control your blood sugar. Lifestyle modifications are the cornerstone of treatment. Leading a healthy lifestyle by exercising, having a diabetic diet, controlling your weight and quitting smoking. These are non-negotiable and are compulsory in the management. The above methods would help you to control your blood sugars, but most patients would need to start medications to bring it back to normal if the sugar levels are very high. The safest margins to keep is a Fasting Blood Sugar of less than 100mg/dl and a HbA1c level which is less than 7% (Ideally less than 6.5%)
Medications that help decrease proteinuria in Diabetic Nephropathy
There are a few medications which help to control proteinuria in a diabetic kidney. A few examples are Enalapril, Ramipril, Losartan, Telmisartan and Valsartan, to name a few common ones. Most diabetic patients with proteinuria would be on one of the above drugs if there are no contraindications to start them. These need to be titrated according to creatinine and the Serum Potassium levels by checking them regularly.
Is Metformin safe in Diabetic
Kidney disease?
It is completely safe in the early stages of Diabetic Nephropathy and only should be stopped by the treating doctor when the kidney function is impaired to a significant degree. This is quite important in treating Diabetes and is a mainstay medication which needs to continue until the treating physician deems it necessary to stop it, according to guidelines or patient factors. Do not stop Metformin on your own as its benefits outweigh the risks most of the time in Diabetic patients. If you are having side effects like bloating, nausea or vomiting, consult your doctor and then stop.
New Medications for Diabetic Kidney Disease
SGLT2 Inhibitors (Sodium-Glucose co-transporter 2) like Empagliflozin and Dapagliflozin are relatively new drugs and are freely available in Sri Lanka now. These medications have been recommended to be started after Metformin or coinciding with it to give the best results to prevent Diabetic Kidney Disease.
GLP1 (Glucagon like peptide-1) agonists are a new class of drugs which are also available in the private sector as Injections or oral medications which have shown benefit in treating Diabetic Kidney Disease. Exenatide and Semaglutide are the known drugs in this class.
High Blood Pressure
Recent studies reveal that nearly 28.2% of adults in Sri Lanka are hypertensive, equating to one in every four adults. The prevalence of hypertension is rising steadily, fuelled by factors such as an aging population and shifting lifestyles. Hypertension, or high blood pressure, refers to the excessive force of blood against the walls of the blood vessels as the heart pumps blood through the body.
A Growing Concern Linked to High Blood Pressure
Our kidneys filter around a litre of blood every minute, removing waste and excess fluid to produce urine. However, high blood pressure can damage the kidneys by constricting blood vessels, reducing blood flow, and impairing their ability to filter waste effectively. This leads to a dangerous cycle where kidney function deteriorates further, contributing to kidney failure. High blood pressure is the second leading cause of kidney failure in Sri Lanka, following diabetes.
Risk factors for hypertension
Age: Individuals over 65 years are more prone to developing high blood pressure due to the natural stiffening of the blood vessels.
Obesity: Excess weight and unhealthy eating habits increase the likelihood of hypertension.
Family History: Those with parents who have high blood pressure are more likely to develop the condition themselves.
Unhealthy Habits: Excessive salt intake, alcohol consumption, physical inactivity, and poor sleep can all elevate blood pressure.
Stress: Chronic stress has also been linked to high blood pressure.
The Importance of Blood
Pressure Screening
Experts recommend that adults aged 40 and older without a history of hypertension check their blood pressure annually by your doctor. For those aged 18-39 with no risk factors, a check-up every 2 to 5 years is advised. Individuals with a family history of hypertension or those at higher risk should undergo more frequent screenings.
Preventing Kidney Damage from High Blood Pressure
The most effective way to prevent or slow the progression of kidney disease caused by hypertension is to keep blood pressure under control. This can be achieved through a combination of medication and lifestyle changes, such as: Take prescribed medications consistently to manage blood pressure. Being physically active, with at least 150 minutes of moderate-intensity exercise per week. Maintaining a healthy weight (BMI between 18.5 and 22.9).Quitting smoking and alcohol consumption. Managing stress through relaxation techniques or therapy. Eating a healthy diet, which includes a reduction in sodium intake and an increase in fruits and vegetables.
It is essential to note that the medications prescribed for high blood pressure do not cause kidney damage. On the contrary, failing to control blood pressure through medications can lead to irreversible kidney damage.
How Urological Issues Can Lead to Chronic Kidney Disease
Conditions such as kidney stones, prostate enlargement and recurrent urosepsis can lead to long-term kidney damage if left untreated.
What are kidney stones?
Kidney stones are solid masses or crystals that form from substances (like minerals, acids and salts) in your kidneys. They can be as small as a grain of sand or rarely larger than a golf ball. Kidney stones are also called renal calculi or nephrolithiasis.
What are the symptoms of kidney stones?
The most common symptom of kidney stones is pain in your lower back, belly or side. It might feel like it extends from your groin to your side. It can be a dull pain or sharp and severe. It’s sometimes called colicky pain because it can get worse in waves.
Other symptoms include: Nausea and vomiting, blood in your pee, pain and inability to pee, feeling the urge to urinate a lot, fever or chills, cloudy or foul-smelling pee.
What causes kidney stones?
Your pee contains minerals, acids and other substances, like calcium, sodium, oxalate and uric acid. When you have too many particles of these substances in your pee and too little liquid, they can start to stick together, forming crystals or stones.
What factors increase the risk for kidney stones?
Not drinking enough fluids, Eating foods high in sodium or sugars, Taking vitamin C supplements and having a family history of kidney stones.
How are kidney stones diagnosed?
Urine test: To see blood, stone-forming crystals in urine and signs of infection.
Imaging: X-rays, CT scans and ultrasound to see the size, shape, location and number of stones.
Blood tests: These check your kidney function, detect infections and look for high levels of calcium or other conditions that could lead to stone formation.
How are kidney stones treated?
Medications: If you have a kidney stone that can pass on its own and isn’t causing infection, a provider may prescribe or recommend medications to relax your ureter to help the stones pass. Commonly prescribed medicines include tamsulosin and nifedipine to manage the pain. Even small stones that can pass on their own can be very painful. Ask your doctor before taking over-the-counter painkillers. Some medicines (NSAIDS) can increase the risk of kidney failure.
Kidney stone procedures
If the stone can’t pass on its own or is blocking your urinary tract, a doctor will recommend a procedure to break up and/or remove the stone.
Shockwave lithotripsy: This procedure uses shockwaves to break the stones from the outside of your body. The fragments can move through your urinary tract and out of your body more easily.
Ureteroscopy: This involves inserting a scope through your urethra and bladder and into your ureter and breaking up and removing the stone. The smaller pieces can move through your urinary tract and out of your body more easily.
Percutaneous nephrolithotomy: This procedure involves inserting a tube directly into your kidney through a tiny incision (cut) in your back. An ultrasound probe breaks apart and removes the stones.
Laparoscopic surgery: This involves making a small incision to remove the stone. In some rare cases, your provider might need to perform open surgery (with a larger incision) instead of a laparoscopy.
Can kidney stones go away on their own?
Yes, around 80% of kidney stones can pass on their own. The amount of time it takes for you to pass a kidney stone depends on its size and location. A stone that’s smaller than 4 mm may pass within one to two weeks. It’s important to follow up with your healthcare provider if you don’t pass the stone within four to six weeks
Can kidney stones be prevented?
Stay Hydrated. Drinking at least 2 to 3 liters of water daily dilutes urine, reducing the risk of stone formation. Limiting foods high in sugar and sodium. Limiting foods high in oxalates. Maintaining a weight that’s healthy for you.Eating foods that are good sources of calcium.
Benign Prostatic Hyperplasia
Benign prostatic hyperplasia (BPH) is a condition in which your prostate grows in size. Your prostate is a gland that rests below your bladder and in front of your rectum. It’s about the size of a walnut, and it surrounds part of your urethra.
What are the warning signs of benign prostatic hyperplasia?
Frequent or urgent need to pee, Peeing more often at night, Trouble starting to pee, Weak urine stream, or a stream that stops and starts, Dribbling at the end of urination, Not being able to fully empty the bladder.
Complications of an enlarged prostate can include: Not being able to pee, This is also called urinary retention.Urinary tract infections (UTIs), Bladder stones can block the urine flow, Kidney damage, Pressure in the bladder from not being able to pee can damage the kidneys or let bladder infections reach the kidneys.
Tests and diagnosis
Prostate-specific antigen (PSA) blood test. PSA is a protein made in the prostate. PSA levels go up when the prostate becomes enlarged. Urinary flow test. You pee into a container attached to a machine. The machine measures how strong your urine flow Ultrasound Scan with Post-void residual volume test. This test measures whether you can empty your bladder fully. Prostate biopsy. This test uses ultrasound imaging to guide needles that take tissue samples of the prostate. Cystoscopy. A lighted, flexible scope is placed into the urethra to see inside the urethra and bladder.
Treatment options
The best treatment choice for you depends on the size of your prostate, your age, your overall health, and how serious your symptoms are. Medications (like Tamsulosin) relax the muscle in your prostate.
Surgeries
Transurethral resection of the prostate (TURP): Your urologist inserts a special instrument (resectoscope) through your urethra that allows them to see and remove prostate tissue.
Transurethral electrovaporisation: Your urologist uses an electrode to heat your prostate tissue. This turns the tissue cells in the enlarged areas of your prostate into steam.
GreenLight laser treatment: Your urologist uses a special laser to evaporate your enlarged prostate tissue.
Aquablation: Your urologist uses precise, high-pressure jets of water to remove prostate tissue.
Conclusion
Chronic Kidney Disease is a silent killer that progresses gradually, often going unnoticed until the late stages. While diabetes and hypertension remain the leading causes, urological conditions such as kidney stones, recurrent urosepsis, and prostate enlargement significantly contribute to kidney damage.
The good news is that CKD caused by these conditions is largely preventable. By adopting a healthy lifestyle, staying vigilant about urinary symptoms, and seeking timely medical intervention, individuals can protect their kidneys and maintain optimal health. Raising awareness about these urological causes of CKD is crucial for early detection and prevention. The key to reducing CKD-related complications lies in education, lifestyle modifications, and regular medical check-ups. Let’s take proactive steps today to safeguard our kidney health for a healthier future.
Source : Daily Mirror




